The 6-step process took about 45 seconds and when coupled with the amount of time a healthcare worker took to remove gloves, go to the dispenser, and let the hands dry, at least a minute will have elapsed.
In a busy emergency department with 10 or more hand hygiene events per hour, personnel might spend 80 to 120 minutes per shift on that activity alone.
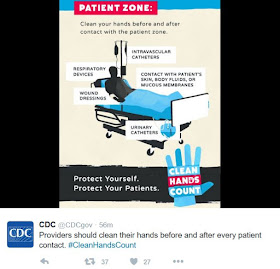
Today is World Hand Hygiene Day and none other than the Centers for Disease Control has validated my hypothesis. Here is what the CDC tweeted today:
An anonymous commenter on my original post said, "Now imagine doing this [the 6-step technique] on rounds, with 40 patients to be seen, and a chief, pgy 3, and 2 interns who have to line up at the sink to do this."
Another commenter named Levi wondered if lower hand colony counts resulted in fewer infections and safer patient care. I don't think that has been investigated.
The CDC also reminded us that hand hygiene must occur before and after
every patient encounter:
As I understand it, the reason hands must be washed after patient contact is that some people contaminate their hands when they remove their gloves. Wouldn't it be simpler and less time-consuming to teach people the correct way to take off gloves? It's not that hard really. Surgeons, scrub techs, and nurses do it every day Maybe it would be better if we washed our hands more often, but took less time to do it.
Thanks to @michelaccad for alerting me to the @CDC tweets.


12 comments:
So you Dr spend all that time washings hands but never clean the tools you use. Things like B/b devices and stereoscopes.
I hope you don't think that's a bad thing. I'm glad they are looking at someone who is fairly balanced on medical reporting.
We don't clean tools. Hospitals have people who do that. Anyway if you mean endoscopes that are contaminated, that is caused by a design flaw that makes them hard to clean.
I doubt that the CDC is really reading my blog, but at least they think the way I do about hand washing.
80-120 minutes per shift devoted to proper hand hygiene? Ooh, sounds like ER wait times are going to increase dramatically. Patients are going to love that, maybe even as much as administrators. Or is this some sort of devious plot to discourage patients from using the ER for primary care and other nonemergent conditions?
It's time that the US faced up to something in healthcare...good, fast, cheap...you can have two but not three. Just let those of us who provide the care which two you want most.
And people ask, "Why don't healthcare workers wash their hands?" Maybe they are too busy at times. I don't see 45 second hand washing rituals catching on.
I am in favor of hand washing,as a tried and true way to prevent pathogen spread. Although, along with hands, I wonder how often providers clean a stethoscope that is used between pts? How many clinicians wear the same lab coat for days without laundering (and then, is it washed with hot water and bleach?)Hospitals should provide scrubs, lab coats, for all and require that employees change into street clothes when they exit. If providers/facilities are serious about not spreading resistant pathogens like VISA/VRSA into the community, then stricter guidelines are required. Imagine what lurks on the soles of healthcare workers' shoes after walking around a hospital all day? Then, those shoes go into public places, not to mention into homes! Along with taking time to wash hands, it takes time to don PPE (personal protective equipment)which are ineffective if not worn correctly every time by every clinician. The topic of infection control is related to the topic of 'preventable events' given that CAUTI and CLABSI are the result of (in many cases) lack of thorough patient hygiene. How many bacteria do you think live on the skin of pts who have not been thoroughly bathed in a week and are incontinent? But administrators would have to hire enough staff to effectively bathe all patients,and that is another story line. So -yes- hospital acquired infections are frequently preventable, but preventative measures cost money. DD
I appreciate your comments. As I have written many times, I think the risk of infection from things like lab coats, ties, phones etc is highly overestimated.
In an ideal world, hospitals should provide scrubs and lab coats that are laundered every day and facilities for all workers to change clothes in. If a hospital has 1000 employees, it would cost quite a bit of money to do that. It's not going to happen.
As far as bathing patients goes, does that even go on in hospitals anymore? The nurses are too busy checking boxes on the computer.
Now that those purple decontamination wipes are everywhere in the ICU, I actually do wipe down my stethoscope after I use it. Those disposable ones kept in the room are a total joke. It is a pure charade when those are used.
I'm still awaiting the first case report of an actual infection proven to be transmitted by a stethoscope or a tie.
I'm still wearing a tie and clean white coat in the office, and my patients compliment me on my appearance. I'm more worried about getting an infection from their clothing than the other way around.
perhaps we really just need to ensure that we, our clothes, and instruments are colonized with "good" bacteria rather than be "sterile" or near sterile.
Artiger, I agree.
Anon, if you figure out how to do that, let me know.
Post a Comment
Note: Only a member of this blog may post a comment.